FAYETTEVILLE, Ark. – A research team led by University of Arkansas chemist Jingyi Chen and University of Arkansas for Medical Sciences microbiologist Mark Smeltzer has developed an alternative therapeutic approach to fighting antibiotic-resistant infections.
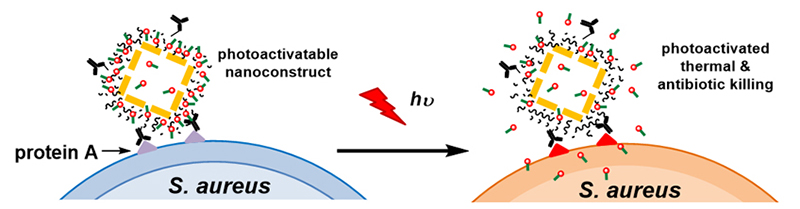
The novel method uses a targeted, light-activated nanodrug consisting of antibiotic-loaded nanoconstructs, which are nanoscale cages made of gold and coated with polydopamine. The antibiotic is loaded into the polydopamine coating. The gold nanocages convert laser irradiation to heat, resulting in the photothermal effect and simultaneously releasing the antibiotic from the polydopamine coating.
.jpg) |
|
Jingyi Chen, University of Arkansas (Photo by University of Arkansas) |
“We believe that this approach could facilitate the effective treatment of infections caused by antibiotic-resistant bacteria, including those associated with bacterial biofilms, which are involved in a wide variety of bacterial infections,” said Chen, assistant professor in the Department of Chemistry and Biochemistry in the J. William Fulbright College of Arts and Sciences.
Microbial resistance to antibiotics has become a growing public health concern in hospitals and the community at large, so much so that the Infectious Diseases Society of America has designated six bacterial species as “ESKAPE pathogens” – Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter species. This designation reflects the limited availability of antibiotics that can be used to treat infections caused by these species.
“It is also estimated that 80 percent of all bacterial infections involve formation of a biofilm, and all of these infections share the common characteristic of intrinsic resistance to conventional antibiotic therapy,” said Smeltzer, professor in the Department of Microbiology and Immunology at UAMS and director of the Center for Microbial Pathogenesis and Host Inflammatory Responses. “Intrinsic resistance refers to the fact that bacteria within a biofilm exhibit a therapeutically relevant level of resistance to essentially all antibiotics”.
Researchers in Smeltzer’s laboratory study the ESKAPE pathogen Staphylococcus aureus. They focus on how the pathogen causes biofilm-associated bone infection and infections associated with orthopaedic implants. But, as Smeltzer explains, there are many other examples in infections – intravenous catheters and vascular grafts, for example – caused by Staphylococcus aureus.
The team used Staphylococcus aureus as the proof-of-principle pathogen to demonstrate the potency of their nanodrug. The combination of achieving a photothermal effect and controlled release of antibiotics directly at the site of infection was achieved by laser irradiation at levels within the current safety standard for use in humans. The therapeutic effects of this approach were validated using planktonic bacterial cultures – bacterial cells that are free-floating rather than contained with a biofilm – of both methicillin-sensitive and methicillin-resistant Staphylococcus aureus strains. However, the method was subsequently shown to be effective even in the context of an intrinsically resistant biofilm.
 |
|
Mark Smeltzer, University of Arkansas for Medical Sciences (Photo by University of Arkansas for Medical Sciences) |
“The even better news is that the technology we developed would be readily adaptable to other bacterial pathogens that cause such infections, including the other ESKAPE pathogens,” Smeltzer said.
The researchers’ work was recently published in ACS Infectious Diseases, a publication of the American Chemical Society (ACS) and “the first journal to highlight chemistry and its role in the multidisciplinary and collaborative field of infectious disease research.”
Participating in the research were first authors Daniel Meeker, an M.D./Ph.D. student in Smeltzer’s lab, and Samir Jenkins, who obtained his doctoral degree in the Chen lab and is now a postdoctoral fellow at UAMS. Other participants included Karen Beenken, senior researcher in Smeltzer’s lab; Allister Loughran at UAMS; Timothy Muldoon, assistant professor of biomedical engineering at the U of A; Amy Powless, doctoral student in biomedical engineering at the U of A; Emily Miller, a U of A undergraduate and Honors College student; Vladimir Zharov, director of the Arkansas Nanomedicine Center at the UAMS Winthrop P. Rockefeller Cancer Institute and professor of otolaryngology, head and neck surgery at UAMS; and Ekaterina Galanzha, associate research professor of otolaryngology, head and neck surgery at UAMS.
About the University of Arkansas: The University of Arkansas provides an internationally competitive education for undergraduate and graduate students in more than 200 academic programs. The university contributes new knowledge, economic development, basic and applied research, and creative activity while also providing service to academic and professional disciplines. The Carnegie Foundation classifies the University of Arkansas among only 2 percent of universities in America that have the highest level of research activity. U.S. News & World Report ranks the University of Arkansas among its top American public research universities. Founded in 1871, the University of Arkansas comprises 10 colleges and schools and maintains a low student-to-faculty ratio that promotes personal attention and close mentoring.
About the University of Arkansas for Medical Sciences: UAMS is the state’s only comprehensive academic health center, with colleges of Medicine, Nursing, Pharmacy, Health Professions and Public Health; a graduate school; a hospital; a northwest Arkansas regional campus; a statewide network of regional centers; and seven institutes: the Winthrop P. Rockefeller Cancer Institute, the Jackson T. Stephens Spine & Neurosciences Institute, the Myeloma Institute, the Harvey & Bernice Jones Eye Institute, the Psychiatric Research Institute, the Donald W. Reynolds Institute on Aging and the Translational Research Institute. It is the only adult Level 1 trauma center in the state. UAMS has 3,021 students, 789 medical residents and two dental residents. It is the state’s largest public employer with more than 10,000 employees, including about 1,000 physicians and other professionals who provide care to patients at UAMS, Arkansas Children’s Hospital, the VA Medical Center and UAMS regional centers throughout the state. Visit www.uams.edu or www.uamshealth.com. Find us on Facebook, Twitter, YouTube or Instagram.
Topics
Contacts
Jingyi Chen, assistant professor, Department of Chemistry and Biochemistry
J. William Fulbright College of Arts and Sciences
479-575-6203,
Mark Smeltzer, professor, Department of Microbiology and Immunology
University of Arkansas for Medical Sciences
501-686-7958,