
Every year, more people die of kidney disease than breast cancer. The Centers for Disease Control and Prevention estimates that 37 million people in the United States — 15% of U.S. adults — have some form of chronic kidney disease.
Of this population, about 100,000 people will develop end-stage renal disease. The treatment options for this group — hemodialysis, peritoneal dialysis or kidney transplant — have not changed significantly over the past 50 years. According to the CDC, the average duration of patient survival on dialysis is approximately seven years, but most patients have to wait 10 years to receive a donated kidney. A hundred thousand people die each year on dialysis, many waiting for a kidney transplant.
Kidney disease is also a major public health problem. The U.S. government spends more than $100 billion in Medicare payments — almost 10% of Medicare’s annual budget of $1 trillion — to care for patients with kidney disease.
A collaboration between engineering researchers at the University of Arkansas and a kidney doctor in Southern California could change all this. If successful, their work will revolutionize treatment for kidney disease and offer hope for something better than dialysis or transplantation.
THE POWER OF ELECTRODEIONIZATION
Several years ago, a decade into his career at the University of Arkansas, chemical engineering professor Jamie Hestekin received a call from Ira Kurtz, a prominent nephrologist in Southern California. Hestekin’s research did not have medical applications, so the call was unexpected and somewhat random. But in other ways, it made perfect sense. At the time, Hestekin had no way of knowing that Kurtz’s call would change the direction of his work and eventually dominate his research agenda.
.jpg) |
| Jamie Hestekin |
Hestekin specializes in a chemical process called electrodeionization, which is why Kurtz was calling. Used primarily in water treatment, electrodeionization removes or separates ions (electrically charged molecules) from water by applying an electrical charge to specially designed membranes.
Before Kurtz’s call, Hestekin had used the technology to remove ions from grape juices, cells from biofuels and organic acids from fermentations. More recently, he was doing consulting research for fracking companies, applying the electrodeionization process to the removal of environmentally hazardous particles from wastewater.
As Distinguished Professor of Medicine and Chief of Nephrology at UCLA Health, Kurtz is a leading basic researcher on the structural biology and physiology of the human kidney. He focuses on proteins that transport various ions in renal and extrarenal tissues. In the kidney, ion transporters play an important role in helping determine the final chemistry of urine.
Kurtz emphasizes that the human kidney is not a simple filter. Rather, it is more like a computer, sensing the chemistry of our blood and keeping it constant, despite all the chemicals that food and beverages introduce into the blood. How the kidney accomplishes this is a major focus of his research.
In addition to studying the ion transport process in the kidney, Kurtz, along with the US Kidney Research Corporation, had been investigating a new, radical idea.
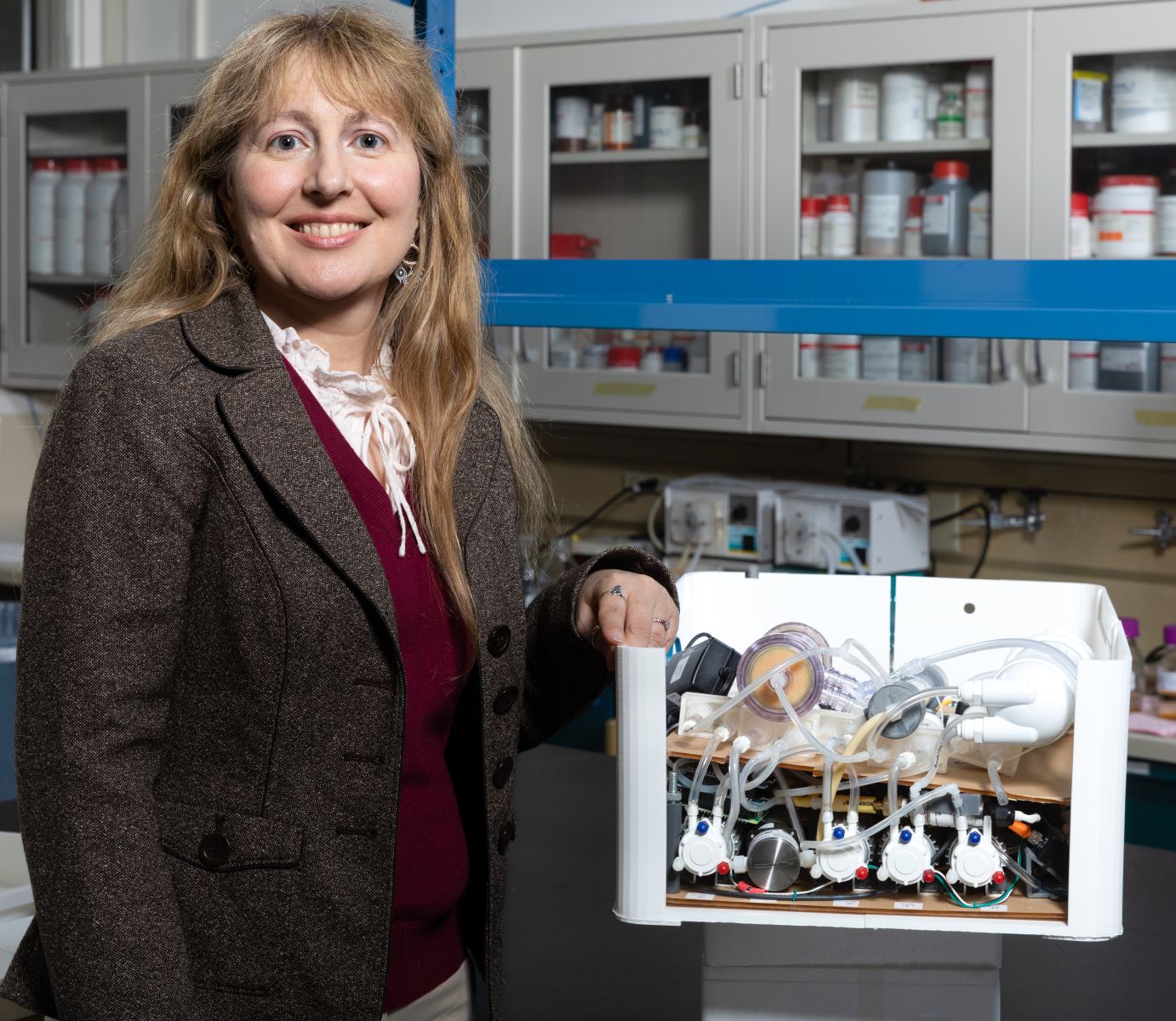 |
| Christa Hestekin |
“I’d been thinking about creating an artificial kidney,” he said. “So, I looked around to see what was out there. There were a few efforts, but I could see they weren’t going to work ultimately. Such a device needed to filter blood, as everyone knew, but compared to the requirement of needing to create a device that could transport ions specifically, the filtration requirement was child’s play.”
Kurtz started exploring techniques that could transport critical ions, such as sodium and potassium, without using dialysis. The device he envisioned would be implantable and therefore couldn’t use water, a dialysate or a dialyzer, which are currently used to treat patients. He ultimately landed on electrodeionization as a technology that could potentially transport ions like the human kidney. After looking at several researchers around the country with a background in this process, Kurtz called Hestekin — because of a paper he had written describing an approach to transporting monovalent cations via electrodeionization.
THE KIDNEY AS A CHEMICAL COMPUTER
Kurtz likes to say that the kidney is more complex than a 747. Weighing in at about a third of a pound, each kidney is located toward the back of the upper abdomen. Its microanatomy is particularly complex, containing roughly a million nephrons, each of which is responsible for filtering and transporting ions and other substances that will end up in the urine. Each nephron contains a filter, called a glomerulus, and a tubular transporting part that is further subdivided anatomically and functionally into about 15 segments that contain different cell types. Kidneys also have nerves, arterial and venous blood vessels, and lymphatics that, along with the nephrons, are configured in a complex three-dimensional structure.
.jpg)
When finished, the artificial kidney will perform all the essential, complex functions of the human kidney.
They never stop working. Despite the fact that people typically eat and drink three times a day, a process that can significantly affect the chemistry of blood and cells, the kidneys recognize these changes and excrete the exact amount of electrolytes, water and organic compounds to compensate for what is absorbed from the human diet into the bloodstream via the gastrointestinal tract. Kidneys prevent the blood chemistry from changing by excreting electrolytes, water and organic substances in urine.
Potassium, one of the many important electrolytes the kidneys regulate, plays a role in the electrical properties of all cells in the body, including cardiac — pacemaker cells that control the heart rate. Unfortunately, in patients without kidney function, whatever they eat and drink stays in their bodies. In such patients, nephrologists need to control what the kidneys would normally do by artificially removing the necessary amount of water and electrolytes during dialysis treatments.
BRIEFCASE-SIZED ARTIFICIAL KIDNEY
Creating an artificial device that performs the above functions is an immense and complex task. The call from Kurtz led to a fruitful collaboration. In addition to Hestekin and Kurtz, the team also includes Christa Hestekin, professor of chemical engineering and associate dean of the Graduate School and International Education, and US Kidney Research Corporation, whose Founder/CEO is Roland Ludlow. Kurtz had established ties with this California-based private company before he knew the Hestekins. US Kidney Research Corporation supports the research and plans to market the world’s first tabletop artificial kidney, based on a prototype that will ultimately be developed by the Kurtz-Hestekin-Ludlow team.
With $4 million in funding from the company, the research team, including students in the Hestekin laboratory, are building a prototype device that fits on a desktop. It could be used at work or placed on a bedside table and used while a patient sleeps.
 |
|
Doctoral student Anelisse Claros demonstrates use of the artificial kidney prototype. |
The device has four basic components that simulate the filtering and critical ion transport functions of an individual nephron. There is an ultrafiltration module that filters blood. Proteins and blood cells return to the patient’s blood, while water, ions, urea and some uremic toxins permeate to the next component in the device. A nanofiltration module helps glucose to return to the blood, while allowing all other substances to permeate. Electrodeionization modules perform the ion transport requirements, and a reverse osmosis module concentrates the synthetic urine and simultaneously controls water excretion, ensuring that the volume of urine approximately matches the patient’s water intake.
Early on, most of the work focused on the electrodeionization module, which selectively removes ions from urine and returns them to the blood. This process was achieved by inserting platinum porous meshes between two ion-exchange wafers to create a single wafer that uses an electric field to force ions through membranes. The meshes serve as electrodes when voltage is applied. This enables independent control of transport chambers within the device, which in turn enables the researchers to select different ions and adjust transport rates independently. The researchers have successfully tested this technology with several physiologically relevant ions, mimicking the specific control of ion transport by the kidney.
More recently, an “accidental” discovery has given the research team further reason to be excited. Ultrafiltration membranes used in hemodialysis, the primary treatment for people with end-stage kidney disease, have problems. They tend to clot. In recent years, in the effort to develop a better membrane, biomedical researchers have focused on the so-called “middle molecule,” that is, design of a membrane that achieves optimal performance in terms of molecule size and electrical charge, one that filters out uremic toxins without losing critical proteins and ions.
As part of a different project, Jamie Hestekin and students in his lab were experimenting with various types of membranes to use as friction material for surface engineering. They were having success with a membrane made of cellulose. Then, a student decided to try it on blood. The results were encouraging.
 |
|
Marcal works with a membrane caster, a machine used for making sheet membranes. |
“This membrane looks more like nature,” Jamie Hestekin says. “It mimics the glomerulus and the tiny fibers connected to it better than anything out there. This was kind of an accidental discovery. We’re still not sure why it mimics the glomerulus better.”
The researchers have used the cellulose membrane in animal studies, but it has not yet been tested as part of the artificial kidney device. The cellulose membrane could potentially be used in hemodialysis dialyzers as well. Its filtering performance is superior to those currently in use, Hestekin says. US Kidney Research Corporation has licensed the membrane for this purpose and is exploring potential collaborations.
WHAT IT MEANS
Developing and marketing an artificial kidney could give patients with kidney disease more options and independence, while potentially reducing Medicare expenditures significantly. Patients using the device would no longer need to go to a dialysis clinic three times a week for treatment. Because their treatment would be done daily at home or in the office, with less stress on the cardiovascular system than three times a week in hemodialysis, there likely would be improvements in both patient quality of life and lifespan.
There’s another major benefit — the environment. Billions of gallons of wastewater produced annually by dialysis treatments would no longer enter water treatment facilities. Development of a waterless artificial kidney would significantly reduce the carbon footprint associated with using and manufacturing water-purifications systems, dialysate solutions and dialyzers. This additional advantage of not using water means the system would be optimal in countries where water is scarce.
The team is also trying to scale down components to create a partially or fully implantable device, which would be about the size of two fists. They first need to complete testing the new filtration membrane and make additional refinements to the tabletop device before creating a protype that can be used in animal trials. The Hestekins and Kurtz estimate this will require an additional $5 million in research funding, and they hope to begin animal trials for the prototype in about 18 months.
.jpg)
Left to right, doctoral student Leticia Santos de Souza, Jamie Hestekin, post-doctoral research fellow Imen Bousrih, post-doctoral fellow Partha Chowdhury and doctoral student Eric Walker.
About the University of Arkansas: As Arkansas' flagship institution, the U of A provides an internationally competitive education in more than 200 academic programs. Founded in 1871, the U of A contributes more than $2.2 billion to Arkansas’ economy through the teaching of new knowledge and skills, entrepreneurship and job development, discovery through research and creative activity while also providing training for professional disciplines. The Carnegie Foundation classifies the U of A among the few U.S. colleges and universities with the highest level of research activity. U.S. News & World Report ranks the U of A among the top public universities in the nation. See how the U of A works to build a better world at Arkansas Research and Economic Development News.
Topics
Contacts
Matt McGowan, science and research communications officer
University Relations
479-575-4246,
dmcgowa@uark.edu