Researchers at the U of A are developing a device that could help medical personnel save lives when they are assessing patients during an emergency.
"This device will determine the dehydration level of patients with minimum delay, such that paramedics and doctors can give the appropriate amount of fluids. This device will help save lives in the ER or in an ambulance," said Robert Saunders, one of the project's developers and an instructor for the Department of Electrical Engineering.
Morten Jensen, a biomedical engineering associate professor, hypothesized with colleagues at the University of Arkansas for Medical Sciences that there is a correlation between venous pressure the pressure within the vein and hydration levels.
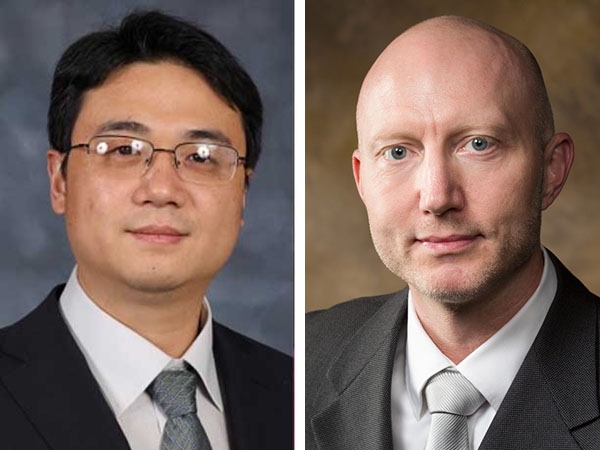
Saunders and Jensen's primary collaborators include Jingxian Wu, professor of electrical engineering, and Dr. Kevin Sexton, associate professor at UAMS. The group is working to develop a device that will help doctors quickly determine a patient's dehydration level at the Arkansas Children's Hospital. They are using data collected from experiments with large animals.
"The dehydration level of a patient is embedded in the shape of venous pressure waves. However, it is difficult to extract such information from the venous pressure waveform, which is usually very weak and buried in noise and interferences. Dr. Wu has developed a new artificial intelligence algorithm that can extract dehydration information from the venous waveform," Saunders said.
Wu, who is working on the signal processing side of the project, said the device uses artificial intelligence to build a correlation between venous pressure and dehydration level.
"We train the model using data collected from patients and animal experiments. The signal processing algorithm can build a model by using the training data, and the model can be used to extract the dehydration information from the venous pressure waveforms."
The device has three potential applications. "The first is for the paramedics in an ambulatory environment. Paramedics can attach an IV to a patient. We can immediately assess the dehydration level of the patient and decide how much fluid the paramedics need to give the patient," Wu explained.
"The second is when a patient is admitted to the ER, particularly pediatric patients. The majority of these patients are actually dehydrated. This shows within the signals of the device. The doctor must assess how much fluid should be kept on hand for the patient. In this traditional setting, determining the level of dehydration requires blood work and can take hours. Often, the doctor needs to decide right away," Wu said.
The third application is on the battlefield when combat soldiers are injured.
"There is blood loss and sometimes internal bleeding. It turns out that dehydration and bleeding have a similar effect on the body. It's still losing fluid. If the medics on the battlefield have this device, they can directly connect it to the soldier to determine whether they are seriously injured. If they are severely dehydrated, it probably means they have severe internal bleeding," Wu said.
However, the device needs more data to improve its accuracy. "The biggest challenge is that we don't have enough data yet. The more data there is to train the machine learning model, the better. We have a limited number of test subjects today," Wu said.
The goal of the interdisciplinary team is to continue to develop the device and have it become a widely used tool in medical emergencies.
Topics
Contacts
Austin Cook, project/program specialist
Department of Electrical Engineering
479-575-7120, ac202@uark.edu
Jennifer P. Cook, director of communications
College of Engineering
479-575-5697, jpc022@uark.edu