By Belinda Watson, Research Intern
What started in a required course at the U of A progressed to a National Science Foundation National Innovation Corps (NSF I-Corps) awardee ($50,000) with the potential for industry application of the Pediatric Spirometry Training Device.
In the fall of 2019, Taylor Farnan enrolled in Clinical Observations and Needs Findings, and would go on to instigate a groundbreaking technology. Clinical Observations and Needs Findings is a required course for students studying biomedical engineering. The purpose of the course is to pair students up with clinicians, depending on their areas of interest, and promote engagement with a variety of different medical environments to pinpoint a need or problem and begin developing a solution, thus preparing students for their senior capstone course. Through this course, Farnan began to work with Dr. Astryd A. Menendez.
Menendez is a pediatric pulmonologist at Arkansas Children's Hospital, and in her experience with the pulmonary function lab, they were struggling to get consistent and accurate data amongst pediatric patients. To gauge lung health, capacity and overall function, doctors administer a spirometry pulmonary function test. The test consists of a patient blowing into a machine, called a spirometer, for six seconds starting with the lungs filled to the top (total lung capacity) with air and exhaling it out to residual volume. But for many pediatric patients, who have never encountered this strange contraption, it is impossible to complete the test. Most pediatric patients can only exhale for three seconds or less, inhibiting accurate evaluations of lung function, resulting in extra visits and tests. Additionally, because it is so difficult to get accurate results from these tests, it is equally as difficult to physiologically assess their lung disease.
At this realization, Farnan began to wonder if she and her team could create a device that would allow patients to prepare for the test, cutting back on extra cost and appointment time. The following spring, in 2019, Farnan recruited Lina Patel, another biomedical engineering student at the U of A, for her technical skills in hardware, software and 3-D printing. With Farnan's idea in mind, the team got to work.
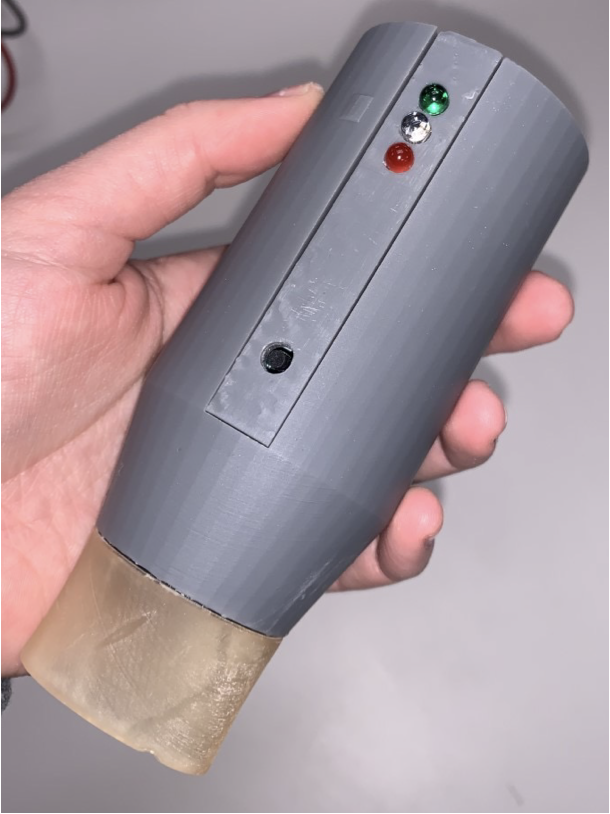
The technology developed quickly through the 2020-2021 school year. The team began developing the device, creating prototypes and testing it out, partnering with electrical engineering students to develop software for their "Pediatric Pulmonary Emission Device." At this point, the device had become the team's senior capstone project, but with graduation fast approaching, neither Patel nor Farnan wanted to leave it behind. They recognized the incredible impact their device could have on testing and diagnostics, and so, they persisted. Nathan Lucas, also a biomedical engineering student at the U of A, then joined the team because of his technical experience and familiarity with the medical device industry.
Looking forward, the team has been accepted into the Summer Cohort No. 1 NSF National I-Corps program and is a recipient of the Chancellor's Commercialization Fund, both totaling $100,000 of follow-on funding investment from the original $300 investment. With this money, the team is hoping to validate their business model and will develop an additional 400 prototypes, enough to allow them to perform a clinical Institutional Review Board study, taking them one step closer to the market.
Farnan is currently at the Georgia Institute of Technology in a Biomedical Innovation and Development Master's program. Amongst other things, she is learning about intellectual property, protecting technology and bringing devices, like their Pediatric Spirometry Training Device, to market. Lucas, who will graduate this spring, plans to continue his education at the University of Kansas in the fall, participating in a similar program. He will continue to support the team through their NSF applications as well as working to bring their device to market. Patel plans to continue at University of Arkansas for Medical Sciences with Menendez, specifically facilitating market application and ensuring clinician interest in the product, which is essential to taking a product to market in the medical field.
The team is advised and supported by industry mentor Ryan Shelton, CEO and co-founder of PhotoniCare Inc.; Morten Jensen, biomedical engineering faculty member and Arkansas Research Alliance Scholar; and Menedez, professor of pediatric and pulmonary medicine in the UAMS College of Medicine Pediatric Pulmonary Section. If the customer discovery results prove to be favorable from the NSF National I-Corps program, the team hopes to apply for the Chancellor's $100,000 GAP Fund, create a new startup company and commercialize their product within the next few years, revolutionizing pediatric pulmonary testing and diagnostics.
Topics
Contacts
Weston Waldo, venture development program manager
Technology Ventures
479-575-5604, waldo@uark.edu
Andy Albertson, senior director of communications
Research and Economic Development
479-575-6111, aalbert@uark.edu