A team of interdisciplinary engineering researchers, in close collaboration with medical professionals, has been awarded a grant from the National Institutes of Health to develop a better way of using images of the heart in surgery planning.
Recent data suggests that in certain cases, nearly one in three surgeries on the heart's mitral valve requires re-operation in the patient's lifetime. Morten Jensen, associate professor of biomedical engineering, and his collaborators hope to reduce that number.
Jensen, along with Jonathan Wenk, associate professor of mechanical engineering at the University of Kentucky, received a three-year, $417,000 grant from the National Institutes of Health Heart, Lung, and Blood Institute to pursue the problem.
The pair are working alongside cardiologists, heart surgeons, cardiothoracic anesthesiologists and the National Center for Toxicology Research Bio-Imaging Laboratory.
Heart failure from problems with the mitral valve comes in two types — one is ischemic, caused by an obstructed coronary artery. The other is caused by degenerative valve disease. Both cause the valve to stop functioning effectively. When the valve fails to close, blood that's supposed to be pumped out through the aorta goes backward to the lungs.
"It's easy enough to get the heart valve to stop leaking, but the difficulty is to get it in a functional shape where a surgical solution will last a long time," Jensen said. "You can put a repair device in it, but that doesn't always give the patient an optimal long-term solution. What we're trying to do is help plan the surgery for longevity. The answer lies with better understanding three characteristics of the heart - the shape, the tissue properties and the amount of stress by the valve in question."
Dr. Drew Rodgers, cardiothoracic anesthesiologist at the Washington Regional Medical Center, said the issue is significant.
"The challenge in our field is to find an optimal solution that solves the problem long-term for all patients," he said.
His colleague, Dr. Charles Cole, heart surgeon at the WRMC Walker Heart Institute, said the opportunity to collaborate with an engineering researcher with a medical background was valuable.
"Dr. Jensen presented his research for our colleagues and invited us to participate," he said. "Being able to communicate with engineers using our own clinical language and have the prospect of being part of such impactful work right here in Northwest Arkansas is very exciting. We can potentially improve the surgical outcome and lives of our own and many other patients across the US and beyond."
Jensen said he was excited about the opportunity to work with local clinical doctors.
"Surgeons plan an operation discussing clinical images with cardiologists, radiologists, or cardiothoracic anesthesiologists, and use their experience to plan the intervention. Making models from these images than can help predict the outcome," Jensen said, "and could be the key to improve the important heart function and secure more long-term effective surgeries."
"These computational models have become more and more prevalent, but they have not been built on a solid foundation in terms of biomechanics," he said. "They've made assumptions about the tissue properties. What we're trying to do is build a set of ground rules for the properties of the tissue."
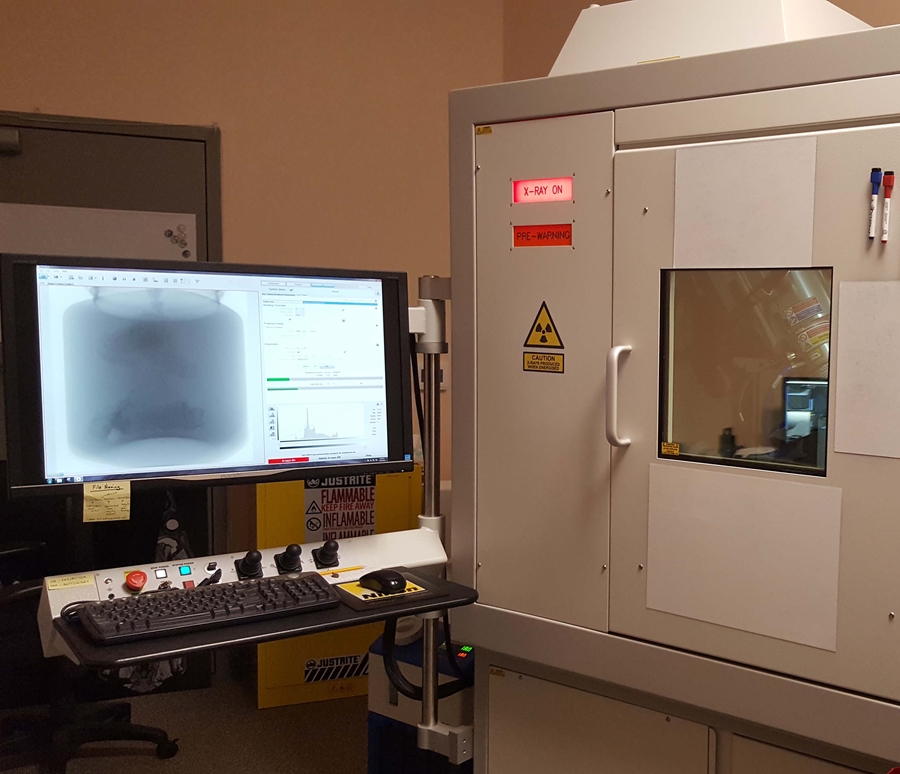
To improve the models, researchers will study pig heart valves, which are similar to human hearts. High-fidelity images of the mitral valve will be taken in collaboration with the Bio-Imaging Laboratory at the National Center for Toxicology Research near Jefferson, Arkansas, building out an accurate profile of its shape. Researchers will then measure the force the valve experiences when the valve closes during the heart cycle. With those two data points, researchers aim to build a more accurate model of the material properties of the heart, which will help doctors better understand conditions when they're preparing for surgery.
"What we do is take both the stress and the shape to point to what the material properties are," Jensen said. "You need to have two components to determine the third component. No one has ever in the past been able to measure the stress in the valve tissue and use that to create the properties of the material for computational models."
With the help of Southeastern Conference travel grants, Jensen and Wenk traveled to the Universities of Kentucky and Arkansas to present the research to mechanical and biomedical engineering faculty members, leading to the collaboration responsible for the current award.
For Jensen, the aim is to improve outcomes for heart failure patients.
"When you go in, you don't expect to have to have heart surgery again," he said.
Topics
Contacts
Morten Jensen, associate professor
Biomedical Engineering
479-575-4216,
Nick DeMoss, director of communications
College of Engineering
479-575-5697,