FAYETTEVILLE, Ark. – Two University of Arkansas engineering professors and an engineering doctoral student have formed Vivas LLC, a new company with licensed technology that can be used to train clinicians in various procedures and test medical imaging equipment.
Vivas has partnered with Humimic Medical LLC, a Fort Smith company that produces medical gels for training, testing and device development. These medical gels are clear or opaque models, made of synthetic gelatin, that accurately simulate human tissue.
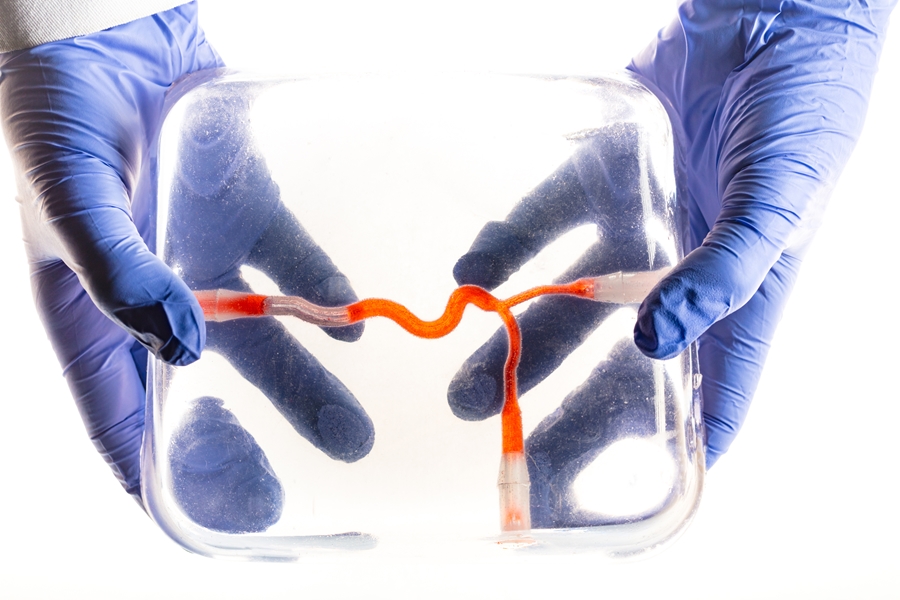
The U of A researchers – Morten Jensen, associate professor of biomedical engineering; Jamie Hestekin, professor of chemical engineering; and Megan Laughlin, a doctoral student in biomedical engineering – used Humimic’s medical gel to create a unique model with small interior channels that simulate human blood vessels. The researchers can pump fluid through these models to simulate blood flow.
 From left, Megan Laughlin, a doctoral student in biomedical engineering. and Morten Jensen, associate professor of biomedical engineering. |
Their technology addresses many clinical training problems – repeated needle sticks on patients by physicians and nurses, for example. Providing models for these practices ensures that equipment works properly and helps build confidence before performing procedures on humans. The medical staff can practice inserting syringe needles into the artificial blood vessels, and the correct positioning of a syringe needle in the blood vessel can be confirmed by the presence of blood-mimicking fluid that enters the syringe from the artificial vessel during the procedure.
The gel models also mimic human tissue in consistency and firmness. They can be transparent for demonstration purposes or opaque, like real tissue, with a variety of skin colors. When an ultrasound transducer is applied to the opaque gel, the ultrasound images appear the same as those taken on the human body. When blood-mimicking fluid is introduced, ultrasound images show multi-colored areas to indicate the presence of this fluid, just as an ultrasound detects blood flow in real human tissue.
“We use models of the human fluid flow system extensively in our cardiovascular biomechanics research laboratory,” Jensen said. “This project was a natural bi-product of those efforts.”
The collaboration with Humimic Medical started because Laughlin and another doctoral student needed realistic models that mimicked human blood vessels. Laughlin’s doctoral projects focus on congenital conditions of restricted flow at the aortic valve and the aorta and how to optimize blood flow with devices. They had worked with a different company to purchase expensive silicon models to perform experiments.
“Using the Humimic gels, we decided we could make these models ourselves, which were more realistic and at a much lower cost,” Laughlin said.
Although the initial purpose of the project was to make artificial blood vessels inside the gel for ultrasound imaging and clinical training, the researchers quickly realized that the combination of their technology and the medical gel could be used to model many aspects of the human body, including organs. The team has begun investigating the possibility of inserting an artificial liver, heart and lungs into gels. They can simulate disease in these organs to test and demonstrate medical equipment and procedures.
The researchers filed an invention disclosure in November 2017, and in January, the University of Arkansas Board of Trustees approved a license agreement for the new technology. Vivas and Humimic Medical started shipping the first products at the end of February. Jensen said the companies have also received international orders, including national government health systems in Europe.
“This industry partnership is already funding university research,” said Hestekin. “It’s our hope that it will also create high-tech jobs in Arkansas in the next couple of years.”
The Office of Industry Engagement assisted with bringing all partners together with the university, and Startup Junkie, a Fayetteville consulting firm focused on innovation and entrepreneurship, provided guidance on company development and strategy.
Funding for the research leading to these technologies was made possible in part by the Arkansas Research Alliance.
“The Arkansas Research Alliance is happy to play a role in seeing this research become a breakthrough in medicine,” said Jerry Adams, president and CEO. “The commercialization of ideas like this are great for Arkansas.”
Jensen is an Arkansas Research Alliance Scholar, and Hestekin holds the Jim L. Turpin Endowed Professorship in Chemical and Biochemical Separations.
Topics
Contacts
Morten Jensen, associate professor, biomedical engineering
College of Engineering
575-4216, mojensen@uark.edu
Megan Laughlin, doctoral student, biomedical engineering
College of Engineering
913-205-0537, mew037@email.uark.edu
Jamie Hestekin, professor, biomedical engineering
College of Engineering
479-575-3492, jhesteki@uark.edu
Matt McGowan, science and research communications officer
University Relations
479-575-4246,
dmcgowa@uark.edu