FAYETTEVILLE, Ark. – An interdisciplinary team of engineers at the University of Arkansas has developed a wireless health-monitoring system that gathers critical patient information, regardless of the patient’s location, and communicates that information in real time to a physician, hospital or the patient herself.
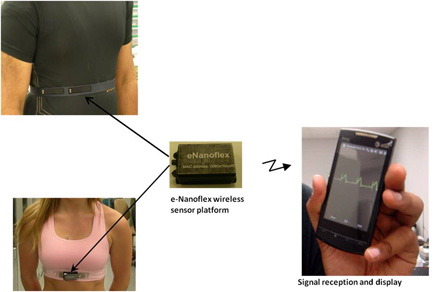
The system includes a series of nanostructured, textile sensors integrated into a conventional sports bra for women and vest for men. Via a lightweight and wireless module that snaps onto these garments, the sensors communicate with system software that relies on a smart phone to collect information, compress it and send it over a variety of wireless networks.
“Our e-bra enables continuous, real-time monitoring to identify any pathophysiological changes,” said Vijay Varadan, Distinguished Professor of electrical engineering. “It is a platform on which various sensors for cardiac-health monitoring are integrated into the fabric. The garment collects and transmits vital health signals to any desired location in the world.”
The system monitors blood pressure, body temperature, respiratory rate, oxygen consumption, some neural activity and all the readings provided by a conventional electrocardiograph (ECG), including the ability to display inverted T waves, which indicate the onset of cardiac arrest. The system does not require a cuff or any extra accessories to measure blood pressure and could therefore replace conventional blood-pressure monitors. It could also replace the cumbersome combination of ECG sensors and wires attached to patients while they walk on treadmills.
The sensors, which are smaller than a dime, include gold nanowires, as well as flexible, conducting textile nanosensors. The sensors are made of arrays of gold nano-electrodes fabricated on a flexible substrate. The textile sensors are woven into the bra material. These sensors do not require conventional sticky electrodes or the use of gel.
Electrical signals and other physiological data gathered by the sensors are sent to the snap-on wireless module, the contents of which are housed in a plastic box that is slightly smaller than a ring box. As the critical wireless component, the module is essentially a low-powered laptop computer that includes an amplifier, an antenna, a printed circuit board, a microprocessor, a Bluetooth module, a battery and various sensors. The size of the module depends heavily on power consumption and minimum battery size. Varadan said that anticipated battery and Bluetooth upgrades will allow the researchers to build a smaller – 1.5 inches long, 0.75 inch wide and 0.25 inch deep – lighter and flexible module that will replace the rigid box.
Data from the sensors then stream to commercially available cell phones and hand-held devices, which expand the use of the system beyond health care. By carrying a cell phone, athletes can monitor all signs mentioned above and other metrics, such as number of calories burned during a workout. To render clean data, the software includes filtering algorithms to mitigate problems due to motion of the hand-held device during exercise.
Whether on a computer or cell phone, the software is set up so that users can view all data on one screen or window, or they can view each measurement on its own unique window. The software also includes a global positioning system that tracks the exact latitude and longitude of the patient or athlete. The geographic information is transferred to a cloud cluster and stored in a secured database that doctors or other health-care personnel can access to view location of the patient as well as historic or real-time ECG data. The system can also be programmed to send emergency messages, via voice or text messaging, if it detects extreme or abnormal conditions.
Varadan has not yet published findings on the e-bra, but results on the system, which he calls an e-Nanoflex Sensor System, were published in the Journal of Nanotechnology in Engineering and Medicine. The research is supported by the Global Institute for Nanotechnology in Engineering and Medicine.
Varadan holds the College of Engineering’s Twenty-First Century Endowed Chair in Nano- and Bio-Technologies and Medicine and the college’s Chair in Microelectronics and High Density Electronics. He is director of the High Density Electronics Center and the Center for Wireless Nano-, Bio- and Info-Tech Sensors and Systems, which is funded by the National Science Foundation. Varadan is also a professor of neurosurgery in the College of Medicine at the University of Arkansas for Medical Sciences in Little Rock, Ark.
Contacts
Vijay Varadan, distinguished professor, electrical engineering
College of Engineering
479-575-2873, vjvesm@uark.edu
Matt McGowan, science and research communications officer
University Relations
479-575-4246,
dmcgowa@uark.edu